- MAC infection is a serious condition that can cause damage to the lungs. MAC infection is not contagious. Common signs and symptoms of MAC lung disease include fatigue, chronic cough, shortness of breath, night sweats, coughing up blood and weight loss. Symptoms may persist or worsen despite being treated for another lung condition.
- If MAC is isolated from a patient who has been started on a three-drug regimen, the clinician may continue the three-drug regimen or switch to the four-drug regimen of INH, EMB, rifabutin, and clofazimine. Although experience is very limited, patients with disease due to M. Kansasii should respond to INH, RIF, and EMB.
- Symptoms Of Mac Lung Disease
- Mac Lung Disease Survival Rate
- Mac Complex Infection
- Syndrome For Cold Hands And Feet
MAC bacteria enter most people's body when inhaled into the lungs or swallowed, but only cause infection in those who are immunocompromised or who have severe lung disease such as those with cystic fibrosis or chronic obstructive lung disease (COPD). Bronchiectasis is a breathing tube (bronchial) disorder characterized by excessive mucus production, cough, and susceptibility to certain infections such as MAC or infection caused by bacteria such as Pseudomonas aeruginosa. Disease in men commonly relates to smoking while disease in women (non-smoking) usually relates to bronchiectasis.
Información en españolTitle

There are 3 types of MAC infections.
- Pulmonary MAC infections - Affect the lungs and are the most common type. These mainly affect elderly women and people who already have lung disease.[2][3]
- Disseminated MAC infections - Have spread throughout the body. This type is usually seen in people with advanced AIDS.[1]
- MAC-associated lymphadenitis - Causes swelling of the
lymph nodes (especially in the neck) and is the most common in young children who have normal immune systems.[3][4]
 While the symptoms are different for each type of infection, general symptoms include fever, night sweats, weight loss, and fatigue. MAC bacteria are found in water, soil, and dust. They infect people when the bacteria are inhaled or swallowed.[1]
While the symptoms are different for each type of infection, general symptoms include fever, night sweats, weight loss, and fatigue. MAC bacteria are found in water, soil, and dust. They infect people when the bacteria are inhaled or swallowed.[1]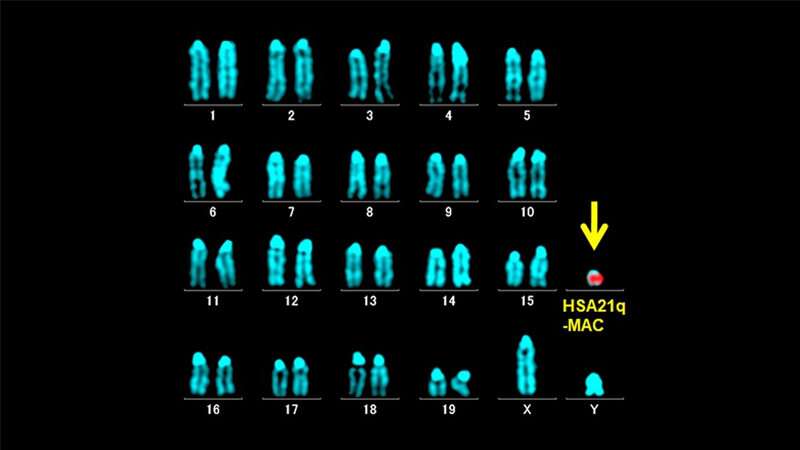 [5] MAC bacteria are not usually spread from person to person. MAC infections are diagnosed by a combination of
[5] MAC bacteria are not usually spread from person to person. MAC infections are diagnosed by a combination of  MAC lymphadenitis causes swollen lymph nodes.[1][2][4]
MAC lymphadenitis causes swollen lymph nodes.[1][2][4]The symptoms of pulmonary MAC infection start slowly, get worse over time and may last for weeks to months. People with pulmonary MAC infections may experience
Symptoms of disseminated MAC infection include: [1][4]
- Fever
- Sweating
- Weight loss
- Fatigue
- Diarrhea
- Shortness of breath
- Abdominal pain
Anemia
There have been a few reports of families with more than one family member with a MAC infection. In these families, it is thought that there is a variation in a
Diagnosis of disseminated MAC infection is suspected based on symptoms and is confirmed in cultures of blood and often
A diagnosis of MAC lymphadenitis is confirmed by finding the bacteria in the culture of lymph node cells. These cells are collected by a
- Pulmonary MAC infection, which affects the lungs
- Disseminated MAC infection, which affects many different parts of the body
- MAC lymphadenitis, which causes swollen
lymph nodes
Treatment options for MAC infections vary by type of infection and by the presence of other medical conditions such as AIDS, cystic fibrosis, COPD, or
For people who have both HIV/AIDS and a MAC infection, treatment usually involves a combination of different antibiotics for the MAC infection and antiretroviral therapy to treat the HIV infection.[1][4]
In special circumstances, there is some evidence to suggest that surgery to remove a single spot of infection in one lung can be helpful in people who have had a poor response to drug therapy. Surgery is usually only done when the infection is found in only one lung and the surgery won't cause any long-term harm.[3][4]
Treatment of MAC lymphadenitis usually involves surgical removal of affected lymph nodes. Antibiotics may also be prescribed depending on the severity of infection and the response to surgery.[3][4]
FDA-Approved Treatments
The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition. Learn more orphan products.- Liposomal amikacin(Brand name: Arikayce) - Manufactured by Insmed Incorporated
FDA-approved indication: September 2018, liposomal amikacin (Arikayce) was approved for the treatment of Mycobacterium avium complex (MAC) lung disease as part of a combination antibacterial drug regimen in patients who do not achieve negative sputum cultures after a minimum of 6 consecutive months of a multidrug background regimen therapy.
National Library of Medicine Drug Information Portal
Medline Plus Health Information
People who are HIV-positive with MAC infections may have a shortened lifespan depending on their immune systems and their response to HIV medications. For people who have had successful treatment, there is still a chance that the infection will come back, so people who have been sick from a MAC infection need to be monitored over time.[2][3]
In HIV-negative people with lung disease from a MAC infection, the treatment success rates range from 20-90% in different studies.[2] People with certain types of lung disease, people who are underweight, and people with
MAC lymphadenitis in children generally does not impact their health. In some cases, the condition may go away even without treatment.[3]
Research helps us better understand diseases and can lead to advances in diagnosis and treatment. The complex download for mac. This section provides resources to help you learn about medical research and ways to get involved.
Clinical Research Resources
- ClinicalTrials.gov lists trials that are related to Mycobacterium Avium Complex infections. Click on the link to go to ClinicalTrials.gov to read descriptions of these studies.
Please note: Studies listed on the ClinicalTrials.gov website are listed for informational purposes only; being listed does not reflect an endorsement by GARD or the NIH. We strongly recommend that you talk with a trusted healthcare provider before choosing to participate in any clinical study.
Support and advocacy groups can help you connect with other patients and families, and they can provide valuable services. Many develop patient-centered information and are the driving force behind research for better treatments and possible cures. They can direct you to research, resources, and services. Many organizations also have experts who serve as medical advisors or provide lists of doctors/clinics. Visit the group’s website or contact them to learn about the services they offer. Inclusion on this list is not an endorsement by GARD.
Organizations Supporting this Disease
- NTM Info & Research (supports pulmonary NTM infections)
550 Madruga Avenue, Suite 230
Coral Gables, FL 33146
Telephone: 305-667-6461, ext 26 and 32
E-mail: ntmmail@ntminfo.org
Website: http://www.ntminfo.org/
These resources provide more information about this condition or associated symptoms. The in-depth resources contain medical and scientific language that may be hard to understand. You may want to review these resources with a medical professional.
Where to Start
- The National Organization for Rare Disorders (NORD) has a report for patients and families about this condition. NORD is a patient advocacy organization for individuals with rare diseases and the organizations that serve them.
In-Depth Information
- Medscape Reference provides information on this topic. You may need to register to view the medical textbook, but registration is free.
- The Monarch Initiative brings together data about this condition from humans and other species to help physicians and biomedical researchers. Monarch’s tools are designed to make it easier to compare the signs and symptoms (phenotypes) of different diseases and discover common features. This initiative is a collaboration between several academic institutions across the world and is funded by the National Institutes of Health. Visit the website to explore the biology of this condition.
- PubMed is a searchable database of medical literature and lists journal articles that discuss Mycobacterium Avium Complex infections. Click on the link to view a sample search on this topic.
- The AIDS Education and Training Center (AETC) offers information on Mycobacterium Avium Complex infections. Click on the link to view this information page.
News
NIH-Supported Research Survey to Examine Impact of COVID-19 on Rare Diseases Community
May 22, 2020
Questions sent to GARD may be posted here if the information could be helpful to others. We remove all identifying information when posting a question to protect your privacy. If you do not want your question posted, please let us know.
Symptoms Of Mac Lung Disease
- Currier JS. Mycobacterium avium complex (MAC) infections in HIV-infected patients. UpToDate. 2017; https://www.uptodate.com/contents/mycobacterium-avium-complex-mac-infections-in-hiv-infected-patients.
- Griffith DE. Overview of nontuberculous mycobacterial infections in HIV-negative patients. UpToDate. 2017; https://www.uptodate.com/contents/overview-of-nontuberculous-mycobacterial-infections-in-hiv-negative-patients.
- Daley CL. Mycobacterium avium Complex Disease. Microbiol Spectr. April, 2017; 5(2):https://www.ncbi.nlm.nih.gov/pubmed/28429679.
- Koirala J. Mycobacterium Avium-Intracellulare. Medscape Reference. 2018; http://emedicine.medscape.com/article/222664-overview.
- Disseminated mycobacterium avium complex disease. US Department of Health and Human Services. 2017; https://aidsinfo.nih.gov/guidelines/html/4/adult-and-adolescent-opportunistic-infection/326/mac.
- Diel R, Lipman M, Hoefsloot W. High mortality in patients with Mycobacterium avium complex lung disease: a systematic review. BMC Infect Dis. 2018; 18(206):1-10. https://bmcinfectdis.biomedcentral.com/track/pdf/10.1186/s12879-018-3113-x.
Newer Therapy Recommended For Treatment-Refractory Mac Pulmonary Inefection
AT A GLANCE
|
ARLINGTON, Va. – A newer therapy that acts like a Trojan horse to attack bacteria should be reserved for patients with certain treatment-refractory lung infections, according to updated nontuberculous mycobacterial (NTM) pulmonary disease guidelines released by the Infectious Diseases Society of America (IDSA), the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the European Society of Clinical Microbiology and Infectious Disease (ESCMID). It is being published in Clinical Infectious Diseases and the European Respiratory Journal.
The therapy, amikacin liposome inhalation suspension (Arikayce®), was approved by the Food and Drug Administration (FDA) in September 2018 to treat people with treatment-refractory Mycobacterium avium complex (MAC), a common cause of NTM pulmonary disease. The antibiotic amikacin is encased in fat globules called liposomes and inhaled into the lungs, where it is released into cells to attack the bacteria. The new IDSA guidelines are in alignment with the FDA that the treatment should only be given to MAC patients who haven’t improved after at least six months of standard therapy.
“Infectious diseases and pulmonary specialists have the expertise to treat these complex NTM pulmonary disease patients, who often require 12-18 months of therapy, sometimes including intravenous treatment,” said Charles L. Daley, MD, lead author of the guidelines and chief of the division of mycobacterial and respiratory infections at National Jewish Health, Denver. “It is likely many patients are being undertreated and others overtreated. The new guidelines should help provide clarity for diagnosis and treatment.”
The new guidelines update the 2007 guidelines, for the first time employing the methodical Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, which specifies the quality and weight of the evidence for diagnosis and treatment. The previous guidelines covered a large amount of material making them complex and difficult to follow. The new guidelines are more focused and provide easier guidance to ensure more patients are treated appropriately, he said.
The guidelines recommend three sputum specimens be obtained at least a week apart and at least two be positive to confirm the person has NTM pulmonary disease. About half of people with the disease do not require antibiotics, at least initially, said Dr. Daley. When it is necessary, treatment typically involves a combination of antibiotics.
Mac Lung Disease Survival Rate
MAC is one of more than 190 species and subspecies of mycobacteria, many of which can cause NTM pulmonary disease in humans and can become chronic. While NTM are found in the environment and can be inhaled, few people develop the disease. However, NTM pulmonary disease has increased from 7 per 100,000 people in 2008 to 12 per 100,00 people in 2015, according to one study. The majority of those with NTM pulmonary disease are women, most of whom are 65 and older and have underlying lung disease.
“Many patients can be cured of the infection, but their underlying lung disease remains incurable,” said Richard J. Wallace Jr., MD, FIDSA, co-author of the guidelines and chairman of the department of microbiology and director of the microbacterial clinical and research laboratory, University of Texas Health Science Center, Tyler. “Other patients can’t be cured of their NTM infection, but can be stabilized with treatment.” Plants vs zombies goty download.
Mac Complex Infection
The guidelines were developed by experts from the United States, Canada, Germany, Italy, Netherlands, France, Spain and Switzerland. In addition to Drs. Daley and Wallace, the guidelines panel was co-chaired by Emmanuelle Cambau, M.D. PhD, and Christoph Lange MD, PhD. Other members of the panel include Jonathan M. Iaccarino, M.D. M.S, Claire Andrejak, M.D. MPH PhD, Erik C. Bottger, M.D., Jan Brozek, M.D. PhD, David E. Griffith M.D., Lorenzo Guglielmetti, M.D.PhD, Gwen A. Huitt, M.D., Shandra L. Knight, MS, Philip Leitman, MBA, Theodore K. Marras, M.D., Kenneth N. Olivier, M.D. MPH, Miguel Santin, M.D. PhD, Jason E. Stout, M.D., Enrico Tortoli ScD, Jakko van Ingen, M.D. PhD, Dirk Wagner, M.D., and Kevin L. Winthrop, M.D.
IDSA has published more than 50 treatment guidelines on various conditions and infections, ranging from HIV/AIDS to skin and soft tissue infections. As with other IDSA guidelines, the NTM pulmonary disease guidelines will be available in a smartphone format and a pocket-sized quick-reference edition.
Note: For a copy of the NTM pulmonary disease guidelines released July 6, 2020, please contact info@idsociety.org.
# # #
The Infectious Diseases Society of America (IDSA), based in Arlington, Va., is a professional society representing more than 12,000 physicians and scientists who specialize in infectious diseases. For more information, visit www.idsociety.org. Follow IDSA on Facebook and Twitter.
Clinical Infectious Diseases is a leading journal in the field of infectious diseases with a broad international readership. The journal publishes articles on a variety of subjects of interest to practitioners and researchers. Topics range from clinical descriptions of infections, public health, microbiology, and immunology to the prevention of infection, the evaluation of current and novel treatments, and the promotion of optimal practices for diagnosis and treatment. The journal publishes original research, editorial commentaries, review articles, and practice guidelines and is among the most highly cited journals in the field of infectious diseases. Clinical Infectious Diseases is an official publication of the Infectious Diseases Society of America (IDSA).
The European Respiratory Journal (ERJ) is the official scientific journal of the European Respiratory Society (ERS) and the most highly regarded peer-reviewed respiratory journal in Europe, with a current impact factor of 11.807. The ERJ features cutting-edge clinical and experimental work in the field of respiratory medicine as well as task force reports and guidelines, reviews and editorials.
About the American Thoracic Society
Founded in 1905, the American Thoracic Society (ATS) is the world's leading medical association dedicated to advancing pulmonary, critical care and sleep medicine. The Society’s more than 16,000 members prevent and fight respiratory disease around the globe through research, education, patient care and advocacy. The ATS publishes four journals, the American Journal of Respiratory and Critical Care Medicine, the American Journal of Respiratory Cell and Molecular Biology, the Annals of the American Thoracic Society and ATS Scholar.
Syndrome For Cold Hands And Feet
The European Society of Clinical Microbiology and Infectious Diseases (ESCMID) (https://www.escmid.org/ ) is the largest European society active in the field of infection with 67 ESCMID-affiliated societies, reaching more than 33,000 clinical/medical microbiologists and infectious diseases specialists in Europe and around the world. ESCMID organizes scientific meetings, educational events, exchange visits between specialists, research and professional matters, issues guidelines, and supported the journal “Clinical Microbiology and Infection” (www.clinicalmicrobiologyandinfection.com).
